The NPUAP/EPUAP guidance on pressure ulcer prevention and treatment should be referred to as best practice in the management of these ulcers (please click on the link below).
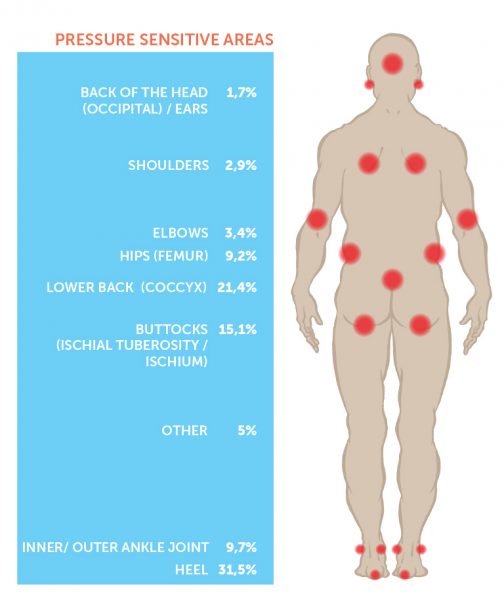
Pressure ulcers occur due to prolonged pressure applied to the soft tissues resulting in completely or partially obstructing the blood flow to the tissues. Pressure ulcers commonly occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. Key areas are the buttocks, heels, hips, ankles, shoulder blades, elbows, knees, back of the head, and ears.
At risk patients
- Immobile patients
- Patients with impaired sensation
- Patients with impaired circulation
- Malnourished patients
- Patients with chronic progressive disorders
- Patients with incontinence
- Older patients, particularly those over 70 years of age
Pressure ulcer prevention
- Understand the risk factors. Identify people who are at risk of pressure ulcers, so that preventative measures can be implemented in the care. There are many risk assessment tools and methods used to assess the level of risk, for instance the Braden Tool, Waterlow Tool and the Norton Tool.
- Thorough, frequent observations of the skin, especially of the bony prominences.
- Plan and document interventions well
- Close follow-up of patients at risk
- Keeping the skin clean and supple, using moisturisers on dry skin and barrier films/creams on areas of skin exposed to excessive moisture
- Correcting nutritional deficiencies, and providing nutritional supplements
- Completely relieve the pressure on the skin at the first sign of skin redness/discolouration
Assessment and reassessment is an integral part of the nurse’s role in pressure ulcer management. Nurses should perform a head to toe skin assessment at least daily, especially checking pressure points such as the sacrum, ischium, trochanters, heels, elbows, and the back of the head using and appropriate assessment tool.
All observations made relating to the skin integrity must be recorded in the nursing documentation, supported by photographs and wound measurements. Pressure relieving equipment must be instigated according to local protocols.